By Ella Hopkins
This blog is one of three, explaining how the coronavirus makes us ill but at differing levels of complexity. This is very much inspired by the format of a brilliant YouTube series by WIRED, with their video explaining how CRISPR works being particularly well made.
If you remember some of the science you learnt at secondary school, this version is for you. (But if you’ve studied biological sciences at higher education level, skip to the next blog instead.)
I mentioned in the Plain English version of this blog that the coronavirus isn’t alive. To understand why viruses infect human cells, it is important to know why they aren’t considered living. There are certain processes only living things do; reproduction is one of these processes. Viruses aren’t alive because they cannot reproduce by themselves, so to make more copies of themselves, they need to infect human cells and take the cell over to make it manufacture the components that make up the virus.
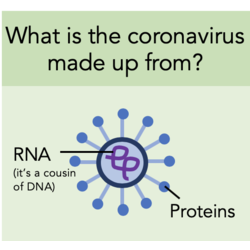
It is known that SARS, that is closely related to the new coronavirus, infects cells in the air sacs (alveoli) of the lungs. It is likely that this is where the coronavirus starts its attack too. The virus infects the cells by making contact between the proteins on its surface and proteins on the surface of the lung cell. This contact, called binding, allows the ‘instructions’ part of the virus into the cell. This ‘instructions’ part is called RNA; it is the chemical cousin of DNA and contains all the information needed to make new copies of the coronavirus.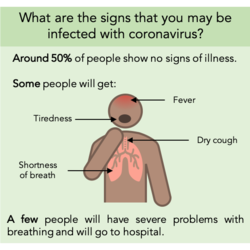
When inside the cell, the coronavirus RNA binds to ribosomes. Ribosomes are tiny ‘factories’ that read the information included in the RNA to make specific proteins. In the case of the coronavirus RNA, the ribosomes are instructed to make lots of proteins that assemble into new coronavirus particles. Once lots of new coronaviruses have been made, they are released from the cell to go and infect more cells. There are some drugs being developed that stop coronavirus from making more copies of itself inside cells. (There should be an article on coronavirus drug development soon to follow, should there be no changes in my working from home conditions.)
With more cells infected, some cells die and alveoli collapse, stopping oxygen being taken into the blood, and CO2 moving out of the blood. Dead cells cause irritation and swelling in the airways - a dry cough is the body’s attempt to move it out of the lungs to be swallowed. Coughing also spreads the coronavirus in droplets in the air, to be inhaled by other people.
Fortunately, the immune system is at hand to help the body fight off coronavirus infection. The immune system is made up of many types of specialised cells. Their main role is to recognise viruses as foreign to the body and kill them. Some immune cells (B cells) release special molecules called antibodies that bind to the virus’ proteins and marks them as a target for other immune cells (phagocytes) to breakdown. There are also immune cells (T cells) that release chemicals called cytokines to warn other nearby immune cells that they have found a virus invader. In some cases, though, immune cells release the wrong chemicals and this can send the immune system into overdrive.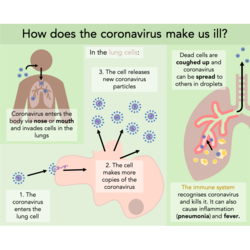
When the immune system response is either too severe, or not severe enough, the balance can tip from the body winning the battle against the coronavirus to the coronavirus winning. The immune system acting too severely can lead to swelling of the lungs (viral pneumonia). This can be very dangerous and cause the lungs to no longer function properly. At this point hospitalisation is often required and respirators can be used to make sure enough oxygen gets into the blood when the lungs are not able to do this efficiently.
I hope you found this informative! If you would like any further explanation of any points, please comment after the blog and I will get back to you.
(To see that last graphic in more detail, use this link to a version on Twitter.)
